The "super-toxic" strain is a mutant form of two E. coli bacteria
Dangerous enterohemorrhagic bacteria E. coli
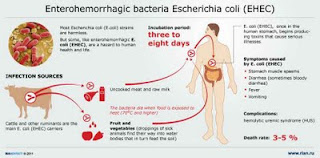
Because, experts say there are gaps in the food safety system, and that it's impossible to test for every illness-causing strain of E. coli. There are no regulations in place today that would prevent this kind of outbreak from occurring. You never know what's around the corner that's just waiting to bite you. E. coli is incredibly common. Hundreds of strains, most of them harmless, live in the intestines of humans, cows and numerous other animals. But some produce toxins that can cause diarrhea, sometimes severe enough to trigger kidney failure, even death.
In Europe's unusually large outbreak, an emerging super-strain named O104:H4 has sickened at least 1,600 people and killed 18. Genetic sequencing suggests that the "super-toxic" strain is a mutant form of two E. coli bacteria, with aggressive genes that could explain the size and lethality of the outbreak. So far, the outbreak is the third-largest involving E. coli in recent world history, and possibly the deadliest. Twelve people died in a 1996 Japanese outbreak that reportedly sickened more than 9,000, and seven died in a 2000 Canadian outbreak.
The most dangerous form in the U.S. has been the E. coli O157:H7 strain, notorious since a 1993 outbreak at a fast-food chain led to its classification as an adulterant in meat, requiring testing and recalls. A 2006 outbreak in spinach highlighted the threat to fresh produce, too. The CDC estimates that strain alone causes about 63,000 foodborne illnesses a year.
original infographics:
E. Coli
Frequently Asked Questions
What is Escherichia coli O157:H7?
How is E. coli O157:H7 spread?
What illness does E. coli O157:H7 cause?
How is E. coli O157:H7 infection diagnosed?
How is the illness treated?
What are the long-term consequences of infection?
What can be done to prevent the infection?
Escherichia coli O157:H7 is an emerging cause of foodborne illness. An estimated 73,000 cases of infection and 61 deaths occur in the United States each year. Infection often leads to bloody diarrhea, and occasionally to kidney failure. Most illness has been associated with eating undercooked, contaminated ground beef. Person-to-person contact in families and child care centers is also an important mode of transmission. Infection can also occur after drinking raw milk and after swimming in or drinking sewage-contaminated water. Consumers can prevent E. coli O157:H7 infection by thoroughly cooking ground beef, avoiding unpasteurized milk, and washing hands carefully.Because the organism lives in the intestines of healthy cattle, preventive measures on cattle farms and during meat processing are being investigated.
What is Escherichia coli O157:H7?
E. coli O157:H7 is one of hundreds of strains of the bacterium Escherichia coli. Although most strains are harmless and live in the intestines of healthy humans and animals, this strain produces a powerful toxin and can cause severe illness. E. coli O157:H7 was fi rst recognized as a cause of illness in 1982 during an outbreak of severe bloody diarrhea; the outbreak was traced to contaminated hamburgers. Since then, most infections have come from eating undercooked ground beef. The combination of letters and numbers in the name of the bacterium refers to the specifi c markers found on its surface and distinguishes it from other types of E. coli.
How is E. coli O157:H7 spread?
The organism can be found on a small number of cattle farms and can live in the intestines of healthy cattle. Meat can become contaminated during slaughter, and organisms can be thoroughly mixed into beef when it is ground. Bacteria present on the cow’s udders or on equipment may get into raw milk. Eating meat, especially ground beef, that has not been cooked suffi ciently to kill E. coli O157:H7 can cause infection. Contaminated meat looks and smells normal. Although the number of organisms required to cause disease is not known, it is suspected to be very small. Among other known sources of infection are consumption of sprouts, lettuce, salami, unpasteurized milk and juice, and swimming in or drinking sew- age-contaminated water. Bacteria in diarrheal stools of infected persons can be passed from one person to another if hygiene or handwashing habits are inadequate.This is particularly likely among toddlers who are not toilet trained. Family members and playmates of these children are at high risk of becoming infected. Young children typically shed the organism in their feces for a week or two after their illness resolves. Older children rarely carry the organism without symptoms.
What illness does E. coli O157:H7 cause?
E. coli O157:H7 infection often causes severe bloody diarrhea and abdominal cramps; sometimes the infection causes nonbloody diarrhea or no symptoms. Usually little or no fever is present, and the illness resolves in 5 to 10 days. In some persons, particularly children under 5 years of age and the elderly, the infection can also cause a complication called hemolytic uremic syndrome, in which the red blood cells are destroyed and the kidneys fail. About 2%-7% of infections lead to this complication. In the United States, hemolytic uremic syndrome is the principal cause of acute kidney failure in children, and most cases of hemolytic uremic syndrome are caused by E. coli O157:H7.
How is E. coli O157:H7 infection diagnosed?
Infection with E. coli O157:H7 is diagnosed by detecting the bacterium in the stool. Most laboratories that culture stool do not test for E. coli O157:H7, so it is important to request that the stool specimen be tested on sorbitol-MacConkey (SMAC) agar for this organism. All persons who suddenly have diarrhea with blood should get their stool tested for E. coli O157:H7.
How is the illness treated?
Most persons recover without antibiotics or other specifi c treatment in 5-10 days. There is no evidence that antibiotics improve the course of disease, and it is thought that treatment with some antibiotics may precipitate kidney complications. Antidiarrheal agents, such as loperamide (Imodium), should also be avoided. Hemolytic uremic syndrome is a life-threatening condition usually treated in an intensive care unit. Blood transfusions and kidney dialysis are often required. With intensive care, the death rate for hemolytic uremic syndrome is 3%-5%.
What are the long-term consequences of infection?
Persons who only have diarrhea usually recover completely. About one-third of persons with hemolytic uremic syndrome have abnormal kidney function many years later, and a few require long-term dialysis. Another 8% of persons with hemolytic uremic syndrome have other lifelong complications, such as high blood pressure, seizures, blindness, paralysis, and the effects of having part of their bowel removed.
What can be done to prevent the infection?
E. coli O157:H7 will continue to be an important public health concern as long as it contaminates meat. Preventive measures may reduce the number of cattle that carry it and the contamination of meat during slaughter and grinding. Research into such prevention measures is just beginning. Back to Top What can you do to prevent E. coli O157:H7 infection? Cook all ground beef and hamburger thoroughly. Because ground beef can turn brown before disease-causing bacteria are killed, use a digital instant-read meat thermometer to ensure thorough cooking. Ground beef should be cooked until a thermometer inserted into several parts of the patty, including the thickest part, reads at least 160o F. Persons who cook ground beef without using a thermometer can decrease their risk of illness by not eating ground beef patties that are still pink in the middle.
If you are served an undercooked hamburger or other ground beef product in a restaurant, send it back for further cooking. You may want to ask for a new bun and a clean plate, too.
Avoid spreading harmful bacteria in your kitchen. Keep raw meat separate from ready-to-eat foods. Wash hands, counters, and utensils with hot soapy water after they touch raw meat. Never place cooked hamburgers or ground beef on the unwashed plate that held raw patties. Wash meat thermometers in between tests of patties that require further cooking.
Drink only pasteurized milk, juice, or cider. Commercial juice with an extended shelf-life that is sold at room temperature (e.g. juice in cardboard boxes, vacuum sealed juice in glass containers) has been pasteurized, although this is generally not indicated on the label. Juice concentrates are also heated sufficiently to kill pathogens.
Wash fruits and vegetables thoroughly, especially those that will not be cooked. Children under 5 years of age, immunocompromised persons, and the elderly should avoid eating alfalfa sprouts until their safety can be assured. Methods to decontaminate alfalfa seeds and sprouts are being investigated. Drink municipal water that has been treated with chlorine or other effective disinfectants.
Avoid swallowing lake or pool water while swimming. See more information about this. Make sure that persons with diarrhea, especially children, wash their hands carefully with soap after bowel movements to reduce the risk of spreading infection, and that persons wash hands after changing soiled diapers. Anyone with a diarrheal illness should avoid swimming in public pools or lakes, sharing baths with others, and preparing food for others.
For more information about reducing your risk of foodborne illness, visit the US Department of Agriculture’s Food Safety and Inspection Service website at: http://www.fsis.usda.gov. For more advice on cooking ground beef, visit the U.S. Department of Agriculture web site at: http://www.fsis.usda.gov/OA/topics/gb.htm
Content source: National Center for Infectious Diseases/Division of Bacterial and Mycotic Diseases
E. coli 0157:H7
(Escherichia coli 0157:H7 infection)
E. coli 0157:H7 Facts
E. coli 0157:H7 is a gram-negative bacterium that can produce a bloody diarrhea due to toxins it secretes when it infects human intestinal tracts.
The symptoms of E. coli 0157:H7 infection may include a low fever, nausea, vomiting, stomach cramps, and bloody diarrhea.
E. coli 0157:H7 is notorious because it can cause additional complications in children and the elderly; renal failure, anemia, and dehydration especially for children (termed HUS or Hemolytic-uremic syndrome) and spontaneous bleeding, organ failures, and mental changes in the elderly (termed TTP or thrombotic thrombocytopenic purpura). Some of these patients develop disabilities or die.
Diagnosis is definitively made when E. coli 0157:H7 is isolated, usually from the patient's stool, and identified as serotype 0157 by immunologic tests.
Most E. coli 0157:H7 infections resolve spontaneously and require no treatment; however supportive treatment is usually quickly required if the patient becomes dehydrated, anemic, or develops HUS or TTP.
The majority of E. coli 0157:H7 infections have excellent outcomes. If complications develop such as severe dehydration, anemia, HUS or TTP, the outcomes can decline from good to poor quickly.
Prevention consists of eating well cooked foods, especially hamburger, and drinking treated or pasteurized fluids. Avoiding touching or eating any food that may be contaminated with any animal or human waste will help prevent the infection.
There is no E. coli 0157:H7 vaccine available for humans.
What is E. coli?
Escherichia coli (E. coli) are gram-negative bacteria that can survive in an environment with or without air (facultative anaerobes) and, depending on the environment, may or may not produce thin hair-like structures (flagella or pili) that allow the bacteria to move and to attach to human cells. These bacteria commonly live in the intestines of people and animals worldwide. There are many strains (over 700 serotypes) of E. coli. Most of the E. coli are normal inhabitants of the small intestine and colon and do not cause disease in the intestines (non-pathogenic). Nevertheless, these non-pathogenic E. coli can cause disease if they spread outside of the intestines, for example, into the urinary tract (where they cause bladder or kidney infections), or into the blood stream (sepsis). Other E. coli strains (enterovirulent E. coli strains or EEC) cause "poisoning" or diarrhea even though they usually remain within the intestine by producing toxins or intestinal inflammation. There are four to six groups (some researchers combine groups) of E. coli strains that comprise EEC.
EHEC (enterohemorrhagic E. coli)
ETEC (enterotoxigenic E. coli)
EPEC (enteropathogenic E. coli)
EIEC (enteroinvasive E. coli
EAEC (enteroadherent E. coli
EAggEC (enteroaggregative E. coli)
E. coli were first isolated by T. Escherich in 1885 and were named after him. The over 700 serotypes are identified by small antigenic changes in their surface "O" antigens (lipopolysaccharides or molecules on the bacterial surface of gram-negative bacteria), for example E. coli 0157 or E. coli 055. These serotypes are identified by immunological tests. E coli strains are further distinguished by "H" protein antigens (different types of flagella that make the bacteria motile). Consequently, a particular E. coli strain can be identified as H, followed by a number, and this identifier is added to the "O" name; for example, E. coli 0157:H7. Although this name designation seems complicated, researchers and clinicians use these antigenic identifiers to track specific E. coli strains that cause outbreaks of disease.
One particular E. coli strain, E. coli 0157:H7 is notorious for its potential to cause disease in man; the remainder of this article will focus on this E. coli strain.
What is E. coli 0157:H7?
E coli O157:H7 is a serotype of E. coli bacteria that form the predominant members of one group of EEC. This EEC group is termed enterohemorrhagic E. coli or EHEC. Unfortunately, other terms in the medical literature describe this group (VTEC or Vero toxin-producing E. coli and STEC or Shiga toxin-producing E. coli). Research suggests that only a small number of E. coli 0157:H7 are needed to cause infection (ingestion of about 10–100 organisms) instead of the thousands to millions needed for infections by other E. coli serotypes. Infection is aided by adhesive receptors (pili or fimbriae) that attach the bacteria to human intestinal cells. The most problems caused by the bacteria are due to two Shiga toxins, termed Stx 1 and Stx 2 and also termed Vero toxins. (Toxins are chemicals that are produced by the bacteria and that damage human cell.) These toxins are almost identical to toxins produced by another related bacterium, Shigella spp that can damage and kill intestinal cells and occasionally cause anemia, damage to platelets, and death of cells in other organs, especially the kidneys.
E. coli 0157:H7 is a major health problem. It is estimated to cause infection in more than 70,000 individuals a year in the United States, and the U. S. Centers for Disease Control and Prevention (CDC) suggests E. coli 0157:H7 is responsible for the majority of "E. coli" outbreaks in the U. S. It has been reported to cause both large outbreaks as well as outbreaks in small numbers of individuals.
This diarrheal illness was first recognized when the CDC personnel isolated E. coli O157:H7 from patients in two separate outbreaks in Oregon and Michigan. The illnesses were associated with eating hamburgers at the restaurants of a national chain; some patients experienced hemorrhagic colitis (inflammation and bleeding of the colon). Thus, hemorrhagic colitis due to E. coli 0157:H7 is commonly referred to as hamburger disease. Since that time, E. coli 0157:H7 also has been associated with contaminated water, foods, and unpasteurized or incorrectly pasteurized (heat treated) dairy products.
The most recent outbreak (October/November of 2010) occurred in five states (California, Arizona, Colorado, New Mexico and Nevada). The CDC linked the outbreak to Gouda cheese sold and given away as free samples at Costco stores
What are the symptoms of E. coli 0157:H7 infections?
Initial symptoms of E. coli O157:H7 infection
The initial symptoms of E. coli O157:H7 infection usually appear about 3 to 5 days (though occasionally in as few as one day or as many as 10 days) after a person ingests the bacteria; the symptoms include
nausea,
vomiting,
stomach cramps, and
diarrhea that often is bloody.
The person may have a mild fever of about 100 to 101F (37.7 to 38.3 C). These symptoms can be seen in infected children and adults.
Later symptoms E. coli O157:H7 infections
The majority of people (especially normal adults) that get the infection resolve the infection without antibiotics in about five to 7 days. However, some people (about 10% of people infected, especially children under the age of 5 and the elderly) develop more severe signs and symptoms, and these people usually require hospitalization and aggressive treatment. These patients develop the usual symptoms listed above, but do not resolve the infection. They develop symptoms that last longer (at least a week) and, if not treated promptly, the infection may lead to disability or death.
These symptoms or complications fall into three main categories;
Hemorrhagic (bloody) diarrhea: Hemorrhagic (bloody) diarrhea symptoms are an increased amount of blood in the diarrheal stool that does not seem to resolve and is usually accompanied by severe abdominal pain. Although this may resolve within a week, some individuals can develop anemia and dehydration that can cause death.
Hemolytic-uremic syndrome (HUS): Hemolytic-uremic syndrome symptoms of pallor (due to anemia), fever, bruising or nose bleeding (due to destruction of blood platelets that are needed for blood to clot), fatigue, shortness of breath, swelling of the body, especially hands and feet, jaundice, and reduced flow of urine may be seen. HUS symptoms usually develop about 7 to 10 days after the initial diarrhea begins. HUS is the most common cause of kidney failure in children; children under 10 years old are the most likely to develop HUS. E. coli 0157:H7 produces toxins that damage the kidneys and destroys platelets that can lead to kidney failure, excessive bleeding, seizures or death.
Thrombotic thrombocytopenic purpura (TTP): Thrombotic thrombocytopenic purpura is caused by the loss of platelets; however, the symptoms that occur are somewhat different and occur mainly in the elderly. The symptoms are fever, weakness, easy, rapid or "spontaneous" bruising, renal failure, and mental impairment that can rapidly progress to organ failures and death. Until the 1980's, TTP was considered a fatal disease, but since the 1980's, plasma exchange and infusion techniques have reduced the death rate in TTP patients to about 10%.
How is an infection with E. coli 0157:H7 diagnosed?
The diagnosis of E. coli 0157:H7 infection begins with an accurate history, physical exam, and an analysis of a sample of stool from the patient. A presumptive diagnosis is frequently made if the patient has symptoms of bloody diarrhea and a history of being exposed to persons, foods or liquids known to be a source of an E. coli 0157:H7 outbreak.
Because other disease-causing bacteria (for example, Shigella and Salmonella) can give patients similar initial symptoms, a definite diagnosis is based on culture of E. coli 0157:H7 from the patient's sample of stool on special culturing plates that then are tested with antiserum (antibodies) that react only with E. coli O157H7. Not all clinics or hospitals have the diagnostic antiserum, so the testing may take a few days.
Because of the high frequency of outbreaks of E. coli 0157:H7, the CDC in 2009 recommended that all patients being screened for community-acquired diarrheal infections have their stool samples analyzed with antisera for Shiga toxins, the toxins that are produced by E. coli 0157:H7 and a few other bacteria, in addition to having cultures of their stool. This approach may result in faster diagnosis of E. coli )157H7 infections.
Blood tests such as a complete blood count (CBC), and blood levels of electrolytes, platelets, blood urea nitrogen (BUN), and creatinine (blood tests that measure function of the kidney) are performed periodically to look for the development of HUS or TTP.
What is the treatment for E. coli 0157:H7?
Patients, especially healthy adults, often require no treatment for E. coli O157:H7 since many infections are self–limited. Moreover, for the acute diarrheal illness, antibiotics have not proven useful. In fact, some studies have shown that antibiotics may increase the chances of developing HUS (up to 17-fold). This effect is thought to occur because the antibiotic damages the bacteria, causing them to release even more toxin. Most investigators suggest antibiotic use only if a patient is septic, that is, there is evidence that the bacterium has spread to parts of the body other than the intestine. In addition, use of atropine and diphenoxylate (Lomotil), drugs that are commonly used to control diarrhea, may also increase symptoms and trigger complications.
When necessary, treatment includes the replacement of fluids and electrolytes to treat or prevent dehydration. Infection with E. coli 0157:H7 should be treated by a physician especially in children and the elderly. HUS and TTP require complex supportive care (for example, plasma exchange) in the hospital. Patients with kidney failure may need dialysis. Consultation with a critical care specialist is often recommended for the care of patients that develop HUS or TTP.
What are the complications and outcomes of infection with E. coli 0157:H7?
Although these conditions have been presented in the symptoms section, they are presented here again because they are actual complications that can occur after the initial disease begins. Patients without these complications usually have excellent outcomes (prognosis). Individuals who develop the following complications have outcomes that range from good to poor, depending on their overall health and how quickly they are diagnosed, treated, and respond to treatment.
Hemorrhagic diarrhea (hemorrhagic enterocolitis)
The incubation period between exposure to EHEC bacteria, including E. coli O157:H7, and the onset of symptoms is usually 3 to 4 days but may be longer in some individuals. Symptoms of EHEC infection include severe abdominal pain and abdominal tenderness which often is associated with bloody diarrhea. Curiously, there often is little or no fever. The diarrhea typically lasts for 6 to 8 days. Dehydration and blood loss can lead to death in some patients if not corrected early.
Hemolytic-uremic syndrome (HUS)
Hemolytic-uremic syndrome (HUS) is the most worrisome complication of EHEC infection, especially in children, because it is a serious and potentially fatal complication. "Hemolytic" refers to the breakup of red blood cells which leads to anemia. There also is destruction of platelets which leads to low blood levels of platelets (thrombocytopenia), which in turn promotes abnormal bleeding. "Uremic" refers to failure of the kidneys. In addition, problems in the brain with seizures and coma may occur.
Hemolytic-uremic syndrome most commonly affects children under the ages of 10 years and is the most common cause of acute kidney failure in infants and young children. It occurs in about 6% to 10% of hemorrhagic colitis caused by E coli 0157:H7 and usually occurs approximately 7 to 10 days after the onset of diarrhea. Early intervention usually results in better outcomes.
Thrombotic thrombocytopenic purpura (TTP)
Persons infected with E. coli 0157:H7, particularly the elderly, can develop a syndrome similar to HUS called thrombotic thrombocytopenic purpura or TTP with clotting of blood within small blood vessels; anemia due to fragmentation of red blood cells; and a shortage of platelets (thrombocytopenia) that results in easy bruising, neurologic abnormalities, impaired kidney function, and fever. TTP is a serious consequence of E. coli 0157:H7 infection that requires early and aggressive treatment since it results in death in about 10% of all patients who develop it.
How do people get E. coli 0157:H7?
Most commonly, E. coli 0157:H7 comes from eating raw or undercooked ground beef (for example, hamburger) or from drinking raw milk. The bacteria are found in animal feces, particularly cattle feces, and contact with the feces can lead to contamination of many types of food and fluids. In 2010, the FDA recalled several productions of beef, including beef placed in pet food. Less commonly, E. coli O157:H7 can be transmitted from one person to another, usually by direct physical contact..
E. coli 0157:H7 prevention
The CDC recommends the following to prevent infections from E. coli 0157:H7:
Wash hands thoroughly after using the bathroom or changing diapers, and before preparing or eating food. Wash hands after contact with animals or their environments (at farms, petting zoos, fairs, even your own pets in your own yard or house).
Cook meats thoroughly. Ground beef and meat that has been needle-tenderized should be cooked to a temperature of at least 160 F (70 C). It's best to use a thermometer, as color is not a very reliable indicator of "doneness."
Avoid raw milk, unpasteurized dairy products, and unpasteurized juices (like fresh apple cider).
Avoid swallowing water when swimming or playing in lakes, ponds, streams, swimming pools, and backyard "kiddie" pools.
Prevent cross contamination in food preparation areas by thoroughly washing hands, counters, cutting boards, and utensils after they touch raw meat.
In addition, many researchers suggest that hamburgers ordered in a restaurant should be cooked through completely, so that no pink hamburger meat is visible inside. This cooking reduces the chance that E. coli will remain alive in the meat. All foods involved in a recall should be put in the trash. No one should attempt to cook the recalled material and eat it.
Because E. coli 0157:H7 is routinely found in the intestines of cattle, companies have developed a vaccine to reduce the number of these bacteria in cattle. The first vaccine for cattle was FDA approved in 2009. There is no vaccine available for E. coli 0157:H7 in humans.
REFERENCES:
CDC.gov. About E. Coli.
CDC.gov. Escherichia coli O157:H7.
U.S. Food and Drug Administration. BBB - Escherichia coli O157:H7 (EHEC).
Previous contributing author Dennis Lee, MD
source: http://www.medicinenet.com/e_coli__0157h7/
Because, experts say there are gaps in the food safety system, and that it's impossible to test for every illness-causing strain of E. coli. There are no regulations in place today that would prevent this kind of outbreak from occurring. You never know what's around the corner that's just waiting to bite you. E. coli is incredibly common. Hundreds of strains, most of them harmless, live in the intestines of humans, cows and numerous other animals. But some produce toxins that can cause diarrhea, sometimes severe enough to trigger kidney failure, even death.
In Europe's unusually large outbreak, an emerging super-strain named O104:H4 has sickened at least 1,600 people and killed 18. Genetic sequencing suggests that the "super-toxic" strain is a mutant form of two E. coli bacteria, with aggressive genes that could explain the size and lethality of the outbreak. So far, the outbreak is the third-largest involving E. coli in recent world history, and possibly the deadliest. Twelve people died in a 1996 Japanese outbreak that reportedly sickened more than 9,000, and seven died in a 2000 Canadian outbreak.
The most dangerous form in the U.S. has been the E. coli O157:H7 strain, notorious since a 1993 outbreak at a fast-food chain led to its classification as an adulterant in meat, requiring testing and recalls. A 2006 outbreak in spinach highlighted the threat to fresh produce, too. The CDC estimates that strain alone causes about 63,000 foodborne illnesses a year.
original infographics:
E. Coli
Frequently Asked Questions
What is Escherichia coli O157:H7?
How is E. coli O157:H7 spread?
What illness does E. coli O157:H7 cause?
How is E. coli O157:H7 infection diagnosed?
How is the illness treated?
What are the long-term consequences of infection?
What can be done to prevent the infection?
Escherichia coli O157:H7 is an emerging cause of foodborne illness. An estimated 73,000 cases of infection and 61 deaths occur in the United States each year. Infection often leads to bloody diarrhea, and occasionally to kidney failure. Most illness has been associated with eating undercooked, contaminated ground beef. Person-to-person contact in families and child care centers is also an important mode of transmission. Infection can also occur after drinking raw milk and after swimming in or drinking sewage-contaminated water. Consumers can prevent E. coli O157:H7 infection by thoroughly cooking ground beef, avoiding unpasteurized milk, and washing hands carefully.Because the organism lives in the intestines of healthy cattle, preventive measures on cattle farms and during meat processing are being investigated.
What is Escherichia coli O157:H7?
E. coli O157:H7 is one of hundreds of strains of the bacterium Escherichia coli. Although most strains are harmless and live in the intestines of healthy humans and animals, this strain produces a powerful toxin and can cause severe illness. E. coli O157:H7 was fi rst recognized as a cause of illness in 1982 during an outbreak of severe bloody diarrhea; the outbreak was traced to contaminated hamburgers. Since then, most infections have come from eating undercooked ground beef. The combination of letters and numbers in the name of the bacterium refers to the specifi c markers found on its surface and distinguishes it from other types of E. coli.
How is E. coli O157:H7 spread?
The organism can be found on a small number of cattle farms and can live in the intestines of healthy cattle. Meat can become contaminated during slaughter, and organisms can be thoroughly mixed into beef when it is ground. Bacteria present on the cow’s udders or on equipment may get into raw milk. Eating meat, especially ground beef, that has not been cooked suffi ciently to kill E. coli O157:H7 can cause infection. Contaminated meat looks and smells normal. Although the number of organisms required to cause disease is not known, it is suspected to be very small. Among other known sources of infection are consumption of sprouts, lettuce, salami, unpasteurized milk and juice, and swimming in or drinking sew- age-contaminated water. Bacteria in diarrheal stools of infected persons can be passed from one person to another if hygiene or handwashing habits are inadequate.This is particularly likely among toddlers who are not toilet trained. Family members and playmates of these children are at high risk of becoming infected. Young children typically shed the organism in their feces for a week or two after their illness resolves. Older children rarely carry the organism without symptoms.
What illness does E. coli O157:H7 cause?
E. coli O157:H7 infection often causes severe bloody diarrhea and abdominal cramps; sometimes the infection causes nonbloody diarrhea or no symptoms. Usually little or no fever is present, and the illness resolves in 5 to 10 days. In some persons, particularly children under 5 years of age and the elderly, the infection can also cause a complication called hemolytic uremic syndrome, in which the red blood cells are destroyed and the kidneys fail. About 2%-7% of infections lead to this complication. In the United States, hemolytic uremic syndrome is the principal cause of acute kidney failure in children, and most cases of hemolytic uremic syndrome are caused by E. coli O157:H7.
How is E. coli O157:H7 infection diagnosed?
Infection with E. coli O157:H7 is diagnosed by detecting the bacterium in the stool. Most laboratories that culture stool do not test for E. coli O157:H7, so it is important to request that the stool specimen be tested on sorbitol-MacConkey (SMAC) agar for this organism. All persons who suddenly have diarrhea with blood should get their stool tested for E. coli O157:H7.
How is the illness treated?
Most persons recover without antibiotics or other specifi c treatment in 5-10 days. There is no evidence that antibiotics improve the course of disease, and it is thought that treatment with some antibiotics may precipitate kidney complications. Antidiarrheal agents, such as loperamide (Imodium), should also be avoided. Hemolytic uremic syndrome is a life-threatening condition usually treated in an intensive care unit. Blood transfusions and kidney dialysis are often required. With intensive care, the death rate for hemolytic uremic syndrome is 3%-5%.
What are the long-term consequences of infection?
Persons who only have diarrhea usually recover completely. About one-third of persons with hemolytic uremic syndrome have abnormal kidney function many years later, and a few require long-term dialysis. Another 8% of persons with hemolytic uremic syndrome have other lifelong complications, such as high blood pressure, seizures, blindness, paralysis, and the effects of having part of their bowel removed.
What can be done to prevent the infection?
E. coli O157:H7 will continue to be an important public health concern as long as it contaminates meat. Preventive measures may reduce the number of cattle that carry it and the contamination of meat during slaughter and grinding. Research into such prevention measures is just beginning. Back to Top What can you do to prevent E. coli O157:H7 infection? Cook all ground beef and hamburger thoroughly. Because ground beef can turn brown before disease-causing bacteria are killed, use a digital instant-read meat thermometer to ensure thorough cooking. Ground beef should be cooked until a thermometer inserted into several parts of the patty, including the thickest part, reads at least 160o F. Persons who cook ground beef without using a thermometer can decrease their risk of illness by not eating ground beef patties that are still pink in the middle.
If you are served an undercooked hamburger or other ground beef product in a restaurant, send it back for further cooking. You may want to ask for a new bun and a clean plate, too.
Avoid spreading harmful bacteria in your kitchen. Keep raw meat separate from ready-to-eat foods. Wash hands, counters, and utensils with hot soapy water after they touch raw meat. Never place cooked hamburgers or ground beef on the unwashed plate that held raw patties. Wash meat thermometers in between tests of patties that require further cooking.
Drink only pasteurized milk, juice, or cider. Commercial juice with an extended shelf-life that is sold at room temperature (e.g. juice in cardboard boxes, vacuum sealed juice in glass containers) has been pasteurized, although this is generally not indicated on the label. Juice concentrates are also heated sufficiently to kill pathogens.
Wash fruits and vegetables thoroughly, especially those that will not be cooked. Children under 5 years of age, immunocompromised persons, and the elderly should avoid eating alfalfa sprouts until their safety can be assured. Methods to decontaminate alfalfa seeds and sprouts are being investigated. Drink municipal water that has been treated with chlorine or other effective disinfectants.
Avoid swallowing lake or pool water while swimming. See more information about this. Make sure that persons with diarrhea, especially children, wash their hands carefully with soap after bowel movements to reduce the risk of spreading infection, and that persons wash hands after changing soiled diapers. Anyone with a diarrheal illness should avoid swimming in public pools or lakes, sharing baths with others, and preparing food for others.
For more information about reducing your risk of foodborne illness, visit the US Department of Agriculture’s Food Safety and Inspection Service website at: http://www.fsis.usda.gov. For more advice on cooking ground beef, visit the U.S. Department of Agriculture web site at: http://www.fsis.usda.gov/OA/topics/gb.htm
Content source: National Center for Infectious Diseases/Division of Bacterial and Mycotic Diseases
E. coli 0157:H7
(Escherichia coli 0157:H7 infection)
E. coli 0157:H7 Facts
E. coli 0157:H7 is a gram-negative bacterium that can produce a bloody diarrhea due to toxins it secretes when it infects human intestinal tracts.
The symptoms of E. coli 0157:H7 infection may include a low fever, nausea, vomiting, stomach cramps, and bloody diarrhea.
E. coli 0157:H7 is notorious because it can cause additional complications in children and the elderly; renal failure, anemia, and dehydration especially for children (termed HUS or Hemolytic-uremic syndrome) and spontaneous bleeding, organ failures, and mental changes in the elderly (termed TTP or thrombotic thrombocytopenic purpura). Some of these patients develop disabilities or die.
Diagnosis is definitively made when E. coli 0157:H7 is isolated, usually from the patient's stool, and identified as serotype 0157 by immunologic tests.
Most E. coli 0157:H7 infections resolve spontaneously and require no treatment; however supportive treatment is usually quickly required if the patient becomes dehydrated, anemic, or develops HUS or TTP.
The majority of E. coli 0157:H7 infections have excellent outcomes. If complications develop such as severe dehydration, anemia, HUS or TTP, the outcomes can decline from good to poor quickly.
Prevention consists of eating well cooked foods, especially hamburger, and drinking treated or pasteurized fluids. Avoiding touching or eating any food that may be contaminated with any animal or human waste will help prevent the infection.
There is no E. coli 0157:H7 vaccine available for humans.
What is E. coli?
Escherichia coli (E. coli) are gram-negative bacteria that can survive in an environment with or without air (facultative anaerobes) and, depending on the environment, may or may not produce thin hair-like structures (flagella or pili) that allow the bacteria to move and to attach to human cells. These bacteria commonly live in the intestines of people and animals worldwide. There are many strains (over 700 serotypes) of E. coli. Most of the E. coli are normal inhabitants of the small intestine and colon and do not cause disease in the intestines (non-pathogenic). Nevertheless, these non-pathogenic E. coli can cause disease if they spread outside of the intestines, for example, into the urinary tract (where they cause bladder or kidney infections), or into the blood stream (sepsis). Other E. coli strains (enterovirulent E. coli strains or EEC) cause "poisoning" or diarrhea even though they usually remain within the intestine by producing toxins or intestinal inflammation. There are four to six groups (some researchers combine groups) of E. coli strains that comprise EEC.
EHEC (enterohemorrhagic E. coli)
ETEC (enterotoxigenic E. coli)
EPEC (enteropathogenic E. coli)
EIEC (enteroinvasive E. coli
EAEC (enteroadherent E. coli
EAggEC (enteroaggregative E. coli)
E. coli were first isolated by T. Escherich in 1885 and were named after him. The over 700 serotypes are identified by small antigenic changes in their surface "O" antigens (lipopolysaccharides or molecules on the bacterial surface of gram-negative bacteria), for example E. coli 0157 or E. coli 055. These serotypes are identified by immunological tests. E coli strains are further distinguished by "H" protein antigens (different types of flagella that make the bacteria motile). Consequently, a particular E. coli strain can be identified as H, followed by a number, and this identifier is added to the "O" name; for example, E. coli 0157:H7. Although this name designation seems complicated, researchers and clinicians use these antigenic identifiers to track specific E. coli strains that cause outbreaks of disease.
One particular E. coli strain, E. coli 0157:H7 is notorious for its potential to cause disease in man; the remainder of this article will focus on this E. coli strain.
Shiga Toxin-Producing E. coli Infection Facts
Escherichia coli, or E. coli for short, is a very common bacterium. There are hundreds of different strains of E. coli. Some are harmless while others cause serious illness. Non-pathogenic strains of E. coli -- those that do not cause disease -- are normal inhabitants of the intestinal tract in humans and animals. But certain strains of E. coli can cause severe diarrhea and infect the genital and urinary tracts.
Examples of Shiga toxin-producing E. coli outbreaks
The most notorious type of pathogenic E. coli is known as E. coli 0157:H7. The name refers to the chemical compounds found on the surface of the bacterium. This strain was identified in 1982 following an outbreak of diarrhea resulting from the eating of undercooked beef. The 0157:H7 E coli strain belongs to a group of bacteria known as "Shiga toxin-producing" E. coli, or STEC for short. They have also been referred to as verocytotoxic E. coli (VTEC) or enterohemorrhagic E. coli (EHEC). Outbreaks of E. coli 0157:H7-induced illness have been common in recent years. In 2011, a deadly outbreak began in Europe due to a rare strain of E coli, Shiga toxin-producing E. coli O104, or STEC O104, that produces a serious illness similar to that produced by E coli 0157:H7. At the time of the outbreak, which was centered in Germany and related to contaminated vegetables, the STEC 0104 strain had never been identified in the United States.
What is E. coli 0157:H7?
E coli O157:H7 is a serotype of E. coli bacteria that form the predominant members of one group of EEC. This EEC group is termed enterohemorrhagic E. coli or EHEC. Unfortunately, other terms in the medical literature describe this group (VTEC or Vero toxin-producing E. coli and STEC or Shiga toxin-producing E. coli). Research suggests that only a small number of E. coli 0157:H7 are needed to cause infection (ingestion of about 10–100 organisms) instead of the thousands to millions needed for infections by other E. coli serotypes. Infection is aided by adhesive receptors (pili or fimbriae) that attach the bacteria to human intestinal cells. The most problems caused by the bacteria are due to two Shiga toxins, termed Stx 1 and Stx 2 and also termed Vero toxins. (Toxins are chemicals that are produced by the bacteria and that damage human cell.) These toxins are almost identical to toxins produced by another related bacterium, Shigella spp that can damage and kill intestinal cells and occasionally cause anemia, damage to platelets, and death of cells in other organs, especially the kidneys.
E. coli 0157:H7 is a major health problem. It is estimated to cause infection in more than 70,000 individuals a year in the United States, and the U. S. Centers for Disease Control and Prevention (CDC) suggests E. coli 0157:H7 is responsible for the majority of "E. coli" outbreaks in the U. S. It has been reported to cause both large outbreaks as well as outbreaks in small numbers of individuals.
This diarrheal illness was first recognized when the CDC personnel isolated E. coli O157:H7 from patients in two separate outbreaks in Oregon and Michigan. The illnesses were associated with eating hamburgers at the restaurants of a national chain; some patients experienced hemorrhagic colitis (inflammation and bleeding of the colon). Thus, hemorrhagic colitis due to E. coli 0157:H7 is commonly referred to as hamburger disease. Since that time, E. coli 0157:H7 also has been associated with contaminated water, foods, and unpasteurized or incorrectly pasteurized (heat treated) dairy products.
The most recent outbreak (October/November of 2010) occurred in five states (California, Arizona, Colorado, New Mexico and Nevada). The CDC linked the outbreak to Gouda cheese sold and given away as free samples at Costco stores
What are the symptoms of E. coli 0157:H7 infections?
Initial symptoms of E. coli O157:H7 infection
The initial symptoms of E. coli O157:H7 infection usually appear about 3 to 5 days (though occasionally in as few as one day or as many as 10 days) after a person ingests the bacteria; the symptoms include
nausea,
vomiting,
stomach cramps, and
diarrhea that often is bloody.
The person may have a mild fever of about 100 to 101F (37.7 to 38.3 C). These symptoms can be seen in infected children and adults.
Later symptoms E. coli O157:H7 infections
The majority of people (especially normal adults) that get the infection resolve the infection without antibiotics in about five to 7 days. However, some people (about 10% of people infected, especially children under the age of 5 and the elderly) develop more severe signs and symptoms, and these people usually require hospitalization and aggressive treatment. These patients develop the usual symptoms listed above, but do not resolve the infection. They develop symptoms that last longer (at least a week) and, if not treated promptly, the infection may lead to disability or death.
These symptoms or complications fall into three main categories;
Hemorrhagic (bloody) diarrhea: Hemorrhagic (bloody) diarrhea symptoms are an increased amount of blood in the diarrheal stool that does not seem to resolve and is usually accompanied by severe abdominal pain. Although this may resolve within a week, some individuals can develop anemia and dehydration that can cause death.
Hemolytic-uremic syndrome (HUS): Hemolytic-uremic syndrome symptoms of pallor (due to anemia), fever, bruising or nose bleeding (due to destruction of blood platelets that are needed for blood to clot), fatigue, shortness of breath, swelling of the body, especially hands and feet, jaundice, and reduced flow of urine may be seen. HUS symptoms usually develop about 7 to 10 days after the initial diarrhea begins. HUS is the most common cause of kidney failure in children; children under 10 years old are the most likely to develop HUS. E. coli 0157:H7 produces toxins that damage the kidneys and destroys platelets that can lead to kidney failure, excessive bleeding, seizures or death.
Thrombotic thrombocytopenic purpura (TTP): Thrombotic thrombocytopenic purpura is caused by the loss of platelets; however, the symptoms that occur are somewhat different and occur mainly in the elderly. The symptoms are fever, weakness, easy, rapid or "spontaneous" bruising, renal failure, and mental impairment that can rapidly progress to organ failures and death. Until the 1980's, TTP was considered a fatal disease, but since the 1980's, plasma exchange and infusion techniques have reduced the death rate in TTP patients to about 10%.
How is an infection with E. coli 0157:H7 diagnosed?
The diagnosis of E. coli 0157:H7 infection begins with an accurate history, physical exam, and an analysis of a sample of stool from the patient. A presumptive diagnosis is frequently made if the patient has symptoms of bloody diarrhea and a history of being exposed to persons, foods or liquids known to be a source of an E. coli 0157:H7 outbreak.
Because other disease-causing bacteria (for example, Shigella and Salmonella) can give patients similar initial symptoms, a definite diagnosis is based on culture of E. coli 0157:H7 from the patient's sample of stool on special culturing plates that then are tested with antiserum (antibodies) that react only with E. coli O157H7. Not all clinics or hospitals have the diagnostic antiserum, so the testing may take a few days.
Because of the high frequency of outbreaks of E. coli 0157:H7, the CDC in 2009 recommended that all patients being screened for community-acquired diarrheal infections have their stool samples analyzed with antisera for Shiga toxins, the toxins that are produced by E. coli 0157:H7 and a few other bacteria, in addition to having cultures of their stool. This approach may result in faster diagnosis of E. coli )157H7 infections.
Blood tests such as a complete blood count (CBC), and blood levels of electrolytes, platelets, blood urea nitrogen (BUN), and creatinine (blood tests that measure function of the kidney) are performed periodically to look for the development of HUS or TTP.
What is the treatment for E. coli 0157:H7?
Patients, especially healthy adults, often require no treatment for E. coli O157:H7 since many infections are self–limited. Moreover, for the acute diarrheal illness, antibiotics have not proven useful. In fact, some studies have shown that antibiotics may increase the chances of developing HUS (up to 17-fold). This effect is thought to occur because the antibiotic damages the bacteria, causing them to release even more toxin. Most investigators suggest antibiotic use only if a patient is septic, that is, there is evidence that the bacterium has spread to parts of the body other than the intestine. In addition, use of atropine and diphenoxylate (Lomotil), drugs that are commonly used to control diarrhea, may also increase symptoms and trigger complications.
When necessary, treatment includes the replacement of fluids and electrolytes to treat or prevent dehydration. Infection with E. coli 0157:H7 should be treated by a physician especially in children and the elderly. HUS and TTP require complex supportive care (for example, plasma exchange) in the hospital. Patients with kidney failure may need dialysis. Consultation with a critical care specialist is often recommended for the care of patients that develop HUS or TTP.
What are the complications and outcomes of infection with E. coli 0157:H7?
Although these conditions have been presented in the symptoms section, they are presented here again because they are actual complications that can occur after the initial disease begins. Patients without these complications usually have excellent outcomes (prognosis). Individuals who develop the following complications have outcomes that range from good to poor, depending on their overall health and how quickly they are diagnosed, treated, and respond to treatment.
Hemorrhagic diarrhea (hemorrhagic enterocolitis)
The incubation period between exposure to EHEC bacteria, including E. coli O157:H7, and the onset of symptoms is usually 3 to 4 days but may be longer in some individuals. Symptoms of EHEC infection include severe abdominal pain and abdominal tenderness which often is associated with bloody diarrhea. Curiously, there often is little or no fever. The diarrhea typically lasts for 6 to 8 days. Dehydration and blood loss can lead to death in some patients if not corrected early.
Hemolytic-uremic syndrome (HUS)
Hemolytic-uremic syndrome (HUS) is the most worrisome complication of EHEC infection, especially in children, because it is a serious and potentially fatal complication. "Hemolytic" refers to the breakup of red blood cells which leads to anemia. There also is destruction of platelets which leads to low blood levels of platelets (thrombocytopenia), which in turn promotes abnormal bleeding. "Uremic" refers to failure of the kidneys. In addition, problems in the brain with seizures and coma may occur.
Hemolytic-uremic syndrome most commonly affects children under the ages of 10 years and is the most common cause of acute kidney failure in infants and young children. It occurs in about 6% to 10% of hemorrhagic colitis caused by E coli 0157:H7 and usually occurs approximately 7 to 10 days after the onset of diarrhea. Early intervention usually results in better outcomes.
Thrombotic thrombocytopenic purpura (TTP)
Persons infected with E. coli 0157:H7, particularly the elderly, can develop a syndrome similar to HUS called thrombotic thrombocytopenic purpura or TTP with clotting of blood within small blood vessels; anemia due to fragmentation of red blood cells; and a shortage of platelets (thrombocytopenia) that results in easy bruising, neurologic abnormalities, impaired kidney function, and fever. TTP is a serious consequence of E. coli 0157:H7 infection that requires early and aggressive treatment since it results in death in about 10% of all patients who develop it.
How do people get E. coli 0157:H7?
Most commonly, E. coli 0157:H7 comes from eating raw or undercooked ground beef (for example, hamburger) or from drinking raw milk. The bacteria are found in animal feces, particularly cattle feces, and contact with the feces can lead to contamination of many types of food and fluids. In 2010, the FDA recalled several productions of beef, including beef placed in pet food. Less commonly, E. coli O157:H7 can be transmitted from one person to another, usually by direct physical contact..
E. coli 0157:H7 prevention
The CDC recommends the following to prevent infections from E. coli 0157:H7:
Wash hands thoroughly after using the bathroom or changing diapers, and before preparing or eating food. Wash hands after contact with animals or their environments (at farms, petting zoos, fairs, even your own pets in your own yard or house).
Cook meats thoroughly. Ground beef and meat that has been needle-tenderized should be cooked to a temperature of at least 160 F (70 C). It's best to use a thermometer, as color is not a very reliable indicator of "doneness."
Avoid raw milk, unpasteurized dairy products, and unpasteurized juices (like fresh apple cider).
Avoid swallowing water when swimming or playing in lakes, ponds, streams, swimming pools, and backyard "kiddie" pools.
Prevent cross contamination in food preparation areas by thoroughly washing hands, counters, cutting boards, and utensils after they touch raw meat.
In addition, many researchers suggest that hamburgers ordered in a restaurant should be cooked through completely, so that no pink hamburger meat is visible inside. This cooking reduces the chance that E. coli will remain alive in the meat. All foods involved in a recall should be put in the trash. No one should attempt to cook the recalled material and eat it.
Because E. coli 0157:H7 is routinely found in the intestines of cattle, companies have developed a vaccine to reduce the number of these bacteria in cattle. The first vaccine for cattle was FDA approved in 2009. There is no vaccine available for E. coli 0157:H7 in humans.
REFERENCES:
CDC.gov. About E. Coli.
CDC.gov. Escherichia coli O157:H7.
U.S. Food and Drug Administration. BBB - Escherichia coli O157:H7 (EHEC).
Previous contributing author Dennis Lee, MD
source: http://www.medicinenet.com/e_coli__0157h7/
Megjegyzések
Megjegyzés küldése